Book review: Values-Based Commissioning of Health and Social Care
This book was a welcome change from the last review, being quite brief in comparison at 155 pages including the index. This isn't a criticism, it just helps in clearing the decks for other reading and distance learning.
The text is no lightweight, however; and should be mandatory reading for all health and social care personnel. Well maybe not all; but that is part of the problem. The clinical and social care workforce are trained to care. Commissioning (and clinical coding) is something done in another location, by other personnel.
If there is a recurring criticism of public services it is that they are cossetted, protected, removed from many of the financial realities of the world. The book, published in 2012, was written anticipating the structural and financial change brought in by the Coalition government and the need for austerity. Therefore, the public sector and clinical staff are not immune from the vagaries of finance as might be assumed. For the past couple of years I've witnessed the regular shakes of the sieve and heard of the same within local authorities.
Christopher Heginbotham's book provides the background and tensions of commissioning and delivers much needed insight on several fronts by conjoining what so often seems remote. The lesson of the book for me is how distinct finance and commissioning are. I can sum this up as: if person-centred clinicians are concerned with sense-making for and with patients and their families, then commissioning is the sense-making of the available finance. Viewed this way you see the importance of commissioning. Clinicians are concerned with evidence-based care, ethics, the health reforms, outcomes, quality, and of course values. Add to this patient involvement and public engagement and you have a read that opens a field that many clinicians dash by (in the public sector?*) as they manage various clinical priorities.
Chapter 1 and 2 set the scene of values-based commissioning, definitions, the fact-value distinction; and the post-Labour NHS. The health reforms (chapter 3) are central to the text, but despite the date of publication which the author acknowledges there is little loss of significance. The health and social care commissioning landscape is still taking shape, outcomes based commissioning (chapter 9) can make the news as implementation is delayed (Williams, 2013). Chapter 4 describes the seven fat years followed by seven lean years; an excellent overview with the major influences at work, The Wanless Reports and Marmot Review for example. It is salutary in these times to see NPfIT as a footnote, with IT benefits still to be accrued (p.32). The need to respond to the public health challenges are noted (chapter 6), as with the potential mental health impact of climate change.
The book's figures and tables are a great asset, very useful to educate student nurses about commissioning, value and values. There are a couple of references to colour (p.72) in what are black and white - grey illustrations. 'Reading' the diagrams you can follow them. The author's background comes across, as with location and mental health experience. The book is I believe relevant to readers across all sectors. Heginbotham also indicates that the book is one of a series by CUP, and points to Fulford et al. as a sibling. There are a couple of repeated words but otherwise the production is excellent. I was a little surprised to find a catastrophe in the text - catastrophe theory (p.51). It is well deployed in explaining complexity and values. When I say surprised perhaps I would really like to see more on this theme of complexity and emergence, but Mr Heginbotham stays clearly on track.
My bias - Hodges' model - found the following standout points:
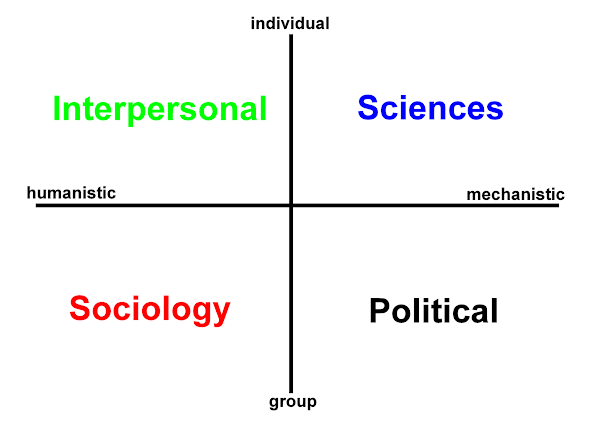
The number of sentences and figures that describe the individual, group, community and population (the structure of Hodges' model). The way that values can act as a counterpoint and essential adjunct to evidence (subjective - objective; qualitative - quantitative).
Some situations are more biological than others - in certain sorts of surgery, for example - and some have a much larger values base - such as in psychiatry (p.40).
Reference to (Cronje and Fullan, 2003):
The medical literature demonstrates an equivocal attitude which suggests a 'collective need to better integrate scientific quantitative data . . . and the art of human judgement . . . into a common definition of "rational" medical practice (p.40).Figure 7.8 Filtering the evidence through a values-based matrix (values across four care domains?).
The use of models to test the real world and reference to a values space.
I posted previously about the nhm - new holistic model (p.80).
(back to the review..!)
Technical aspects (a law and index) and ethical issues that beset commissioning are introduced (space is limited), and recur helping to integrate the book as a whole. Chapter 5 deals with public involvement and engagement and how it can be enacted. Chapter 7 on integrative commissioning invariably raises patient and service user care pathways.
Is this the Rorschach test for patient, care professional and commissioner: please draw your care pathway?
The book admirably deals with the ideal and realised in the space available. As such even when there is a linear care pathway it is how it is experienced that counts (values and outcomes...). (It is sadly the person-affirming life-story pathway that is so often lost.)
Perhaps, this is what I have in mind above in referring to emergence. Despite the existence of care pathways in practice the route in-through health and social care is probably found in a rather chaotic way (sudden care transitions); with delays, placement changes, ward movement(s)-stasis, choices to be taken into account, lack of attendance, missed appointments. ... This is why trying to define pathways may certainly assist, but it is the granularity of those definitions and their experience that snags at our clothes along the way. As Heginbotham advises - care pathways are not something to use in a slavish way. This excellent and well referenced book should provoke and establish interest in this very important health and social care activity. An activity and process that must be informed by the values of the public and those of patients and be more than a process, but realised in shared purposes and practise.
*When we stop and reflect we also recognise ourselves as tax-payers and so seek value-for money, and the other e's of efficiency, effectiveness, efficacy...
Many thanks to CUP for the copy.
Williams, D. Trust forces delay in outcomes based commissioning plan, Health Service Journal, 6 December 2013. p. 4-5.
Heginbotham, C. (2012) Values-Based Commissioning of Health and Social Care. Cambridge, Cambridge University Press.

 orcid.org/0000-0002-0192-8965
orcid.org/0000-0002-0192-8965